Hemopure is used in the treatment of severe autoimmune hemolytic anemia
![]() 2024-07-17
2024-07-17
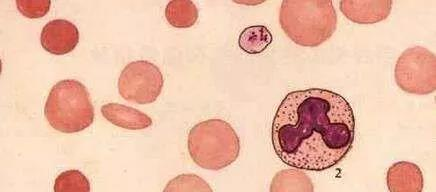
Autoimmune hemolytic anemia (AIHA) is a kind of hemolytic anemia caused by the disorder of immune function in vivo, the production of autoantibodies and/or complement adsorbed on the surface of red blood cells, and the acceleration of red blood cell destruction by antiantigen antibody reaction.
Blood transfusion is one of the common treatment methods for AIHA, but it may also accelerate hemolysis, aggravate anemia, and even cause acute renal failure or disseminated intravascular coagulation, resulting in death. It is especially dangerous when a large amount of blood is transfused. Therefore, blood transfusion should be avoided as far as possible, and washed red blood cells should be transfused when necessary.
Hemoglobin oxygen carriers (HBOC) are a kind of artificial blood substitutes, mainly from human blood, animal blood and recombinant hemoglobin. The most typical HBOC product is HBOC-201, the only polymerized bovine hemoglobin for human use that has ever been approved for marketing in the world ➊. HBOC-201 is a purified, cell-free, and sterile solution of glutaraldehyde polymerized bovine hemoglobin buffered in lactated Ringer's solution. HBOC-201 has a longer shelf life, a lower risk of transfusion-related reactions, and faster oxygen uptake than red-cell transfusions. Previous HBOC studies have focused on patients with major bleeding, and the absence of cell surface antigens in HBOC-201 solution means that it has the potential to play a role in AIHA treatment. The following is an application case of HBOC-201 to cure a lady with severe AIHA.
Case reports:
A 21-year-old woman presented to the hospital with a punctate rash and bleeding gums. Physical examination revealed multiple ecchymosis, and a preliminary diagnosis of idiopathic thrombocytopenic purpura was made. Prednisone was started, and the platelet count immediately increased to 83,000 per cubic millimeter. Twelve days after the initial discharge, the patient was readmitted with dyspnea and fever. Within 12 hours of admission, the hematocrit decreased and ischemic symptoms developed. Transfusion of 2 units of red-cell dense fluid followed by methylprednisolone and intravenous immune globulin resulted in temporary improvement in anemia. Symptoms of hemolysis increased over the next 45 days, and anemia remained intractable after high-dose glucocorticoids, plasmapheresis, splenectomy, and a second course of intravenous immune globulin. Patients require up to eight units of red blood cell thick fluid per day. Fever, nausea, and back pain were initiated at the time of transfusion due to acute hemolysis. At this time, treatment with cyclophosphamide was started.
Because conventional transfusion was ineffective, written informed consent was obtained from the patient to use HBOC-201 as an alternative oxygen-carrying solution until the autoimmune hemolytic anemia resolved. Us Institutional Ethics review boards, the US Army Medical Command, and the FDA have also approved the product for compassionate use.

Treatment Methods and Results:
Patients were infused with HBOC-201 when there was clinical evidence of end-organ ischemia (acid or base excess), hemodynamic decline, or a decrease in the whole-blood hemoglobin level to less than 4 g per deciliter. A total of 11 units of HBOC-201 were infused in seven separate infusions over seven days. No adverse reactions caused by HBOC-201 were found. During HBOC-201 treatment, the mean total hemoglobin level was 5.5g per deciliter (3.4mmol per liter), and the corresponding mean hematocrit was 9.5%. In some cases, hemoglobin levels and hematocrit were nearly equal, suggesting that most of the oxygen-carrying capacity of blood can be attributed to soluble hemoglobin. The patient was discharged in good condition 100 days after completion of HBOC-201 treatment. Eight months after discharge, the patient remained well, with a hematocrit consistently greater than 35%.
Performance and safety of HBOC-201:
Over the past two decades, there has been intense interest in the development of safe and effective alternatives to human red blood cells. Of these, the polymeric form of bovine hemoglobin has shown particularly promise. They have a molecular structure similar to that of human hemoglobin but with a lower concentration of organophosphates and therefore more pronounced oxygen unloading in ischemic tissue and enhanced binding of carbon dioxide and hemoglobin in the deoxygenated state. The affinity of bovine hemoglobin for oxygen is partially regulated by serum chloride, whereas the affinity of human hemoglobin for oxygen is affected by 2, 3-diphosphoglycerate. All these give HBOC-201 excellent oxygen transport properties.
In sheep models, bovine hemoglobin has been shown to maintain tissue oxygen delivery at a hematocrit as low as 2.4% for more than a month. HBOC-201 has been shown to be safe and well tolerated in normal adults and in patients with sickle cell disease. At the same time, it was also studied in vivo in patients undergoing elective abdominal aortic surgery. It is reported that this case is the first use case of HBOC-201 in a patient with severe autoimmune hemolytic anemia.
Infusion of hemoglobin-based solutions is often accompanied by a rise in systemic and pulmonary arterial pressure, which is a sign of vasoconstriction. The reason for this response is the binding of the hemoglobin moiety to nitric oxide. This response has been associated with reduced cardiac output, and some studies have found it to be associated with impaired oxygen delivery. At the time of the initiation of treatment in this case, no traumatic hemodynamic monitoring was performed, and no significant vasoconstrictor response to HBOC-201 was observed. In the case of HBOC-201 infusion in patients with sickle cell disease, there was similarly no hypertensive response. In addition, in the case of patients undergoing abdominal aortic surgery, higher doses of HBOC-201 may have resulted in milder vasoconstriction, and metabolic acidosis reflecting ischemia was also improved with the infusion of HBOC-201.
In conclusion, HBOC-201 as an alternative mediator of oxygen delivery is a boon for patients with refractory autoimmune hemolytic anemia. HBOC-201 can provide strong support for patients with a hematocrit of only 4.4%, and no immediate or long-term ischemic damage occurs. Because HBOC-201 has no cell-surface antigen, this makes it effective in delivering oxygen to patients with severe autoimmune hemolytic anemia.
Note: 1. Hemopure is a glutaraldehyde polymerized bovine hemoglobin product developed by Biopure Company in Cambridge, Massachusetts, USA. It is the representative variety developed by HBOC and the most mature variety at present. Runfang Bio introduces the original Biopure technology, and has complete intellectual property rights, which will open a new page for the research and development, production and application of blood substitutes in China.
Article source:
Transfusions of Polymerized Bovine Hemoglobin in a Patient with Severe Autoimmune Hemolytic Anemia.
John Mullon, M.D., George Giacoppe, M.D., Cynthia Clagett, M.D., David McCune, M.D., and Thomas Dillard, M.D.
-

Bios Wins the “Global Hemoglobin Oxygen Carrier Technology Innovation Leadership Award” at the Sullivan New Investment Conference 2025
On August 27, the 19th Sullivan Global Growth, Technology Innovation and Leadership Summit 2025 and the 4th New Investment Conference (hereinafter referred to as “Sullivan New Investment Conference 2025”) was grandly opened in Shangri-La Hotel, Jing ’an District, Shanghai.
2025-08-29
-

Wang Jianfeng, the Secretary of the CPC Changzhou Municipal Committee, met with Mr. Zheng Zhiheng, the Chairman of Bios Biologics
On 28 May 2025, Wang Jianfeng, Party Secretary of Changzhou City, Jiangsu Province, met with Mr. Zheng Zhiheng, Chairman of Bios Biotechnology Co., LTD., Vice Chairman and Executive Director of Chow Tai Fok Jewelry Group Co., LTD., to exchange views on further deepening cooperation.
2025-05-29
-

Yale scientists have successfully revived a pig brain with artificial blood
Recently, the cover of Nature published the latest research from Yale University School of Medicine: scientists at Yale University used an infusion solution to successfully revive the pig brain after 4 hours of death, restoring some cellular and metabolic functions, and maintaining them for at least 6 hours.
2024-08-03
-
A brief history of research and development of red blood cell substitutes
Blood has always been a very important, but very limited medical resource.
2024-08-02


